Wednesday (8/2), the Center for Medical Bioethics and Humanities held the Raboan Discussion Forum. The topic that we raised was Bioethical Problems in Women’s Surgical Methods of Contraception. The speaker for this discussion was Dr. Annisa Ullya Rasyida, dr., M.Si. and moderated by dr. Tiea Khatija.
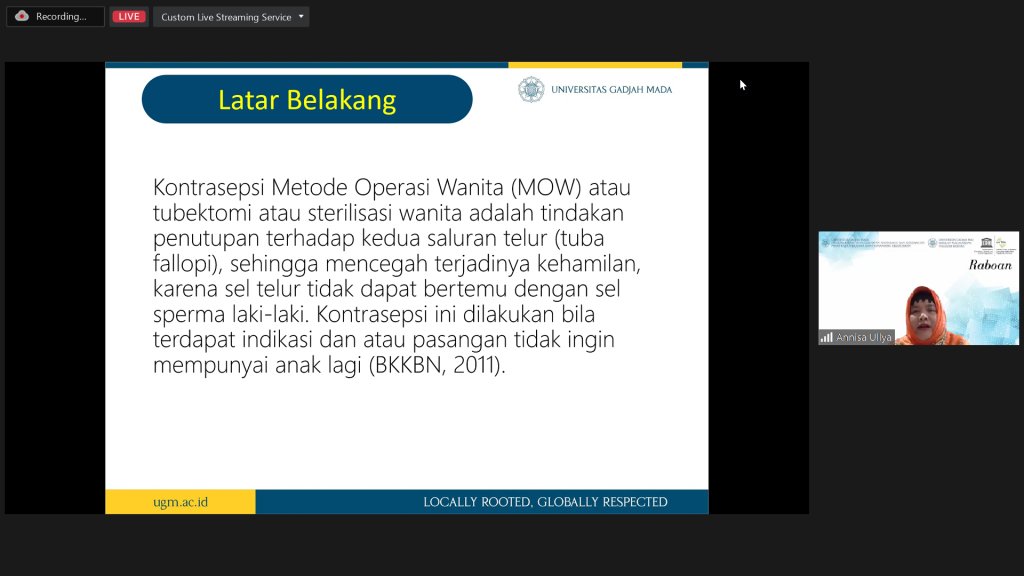
Women’s Surgical Methods of Contraception (MOW) or female tubectomy or sterilization to close the fallopian tubes, to preventing the pregnancy, because the ovum can’t meet sperm cells. Contraception can be done if there are indications and/or the couple doesn’t want to have more children (BKKBN, 2011). One of the indications for someone that use the MOW contraception is the presence of psychological/physical disturbances when the woman is pregnant again. Only 44.5% of MOW acceptors knew about the side effects of using that contraception. MOW contraceptive users can only give birth with caesarean section method is maximum of 3 times. The use of MOW contraception is recommended for mothers who have heart defects that are quite serious.
New Sense of Bioethics:
- Belief in God or Faith: doctors being an intermediator to help patients, but God determines the outcome. Patient like to stubborn, because they feel that death is in God’s hand, so they still want to try.
- Respect for others: doctors respect the wishes of patients and do not force patients to sign informed consent. The patient has been explained the action procedure, but when the formula Is not clearly written and there is a risk, the patient blames the doctor.
- Beneficence: doctor tries to help patient, in this case the patient feels loss in the future because she can’t get pregnant again
- Non maleficence: the doctor tries to save the patient’s life. In this case the patient was saved by being advised to be sterile because he had a history of the disease. But, turns out patient wants to get pregnant again and she knows that she can’t, the patient feels aggrieved.
- Social justice for all: doctors help patients regardless of status.
The absence of the word “permanent sterile” on the informed consent sheet make an opportunity to bring the matter into the realm of law. The response: verbal consent is sufficient, so written informed consent is only a confirmation of what has been previously agreed upon. However, it would be better if the informed consent was written in full of the purpose, benefits and risks of an action/operation. Then effective communication builds trust between doctors and patients.
Writer: Safirra Afifah Firanka
Watch full video here






